Take two. Scientists recreate stem cells in the lab by turning back the clock in skin cells (fibroblasts) obtained by skin biopsy. These reprogrammed cells are referred to as induced pluripotent stem (iPS) cells. Video: Genetics Policy Institute.
Researchers are working hard to discover and develop medicines for ALS. But with four drugs dropping out of the pipeline at phase II or III in the last nine months alone, a growing number of scientists are thinking outside of the model box in hopes to identify more effective medicines for the disease.
One emerging strategy is to use stem cell-based reprogramming technologies to develop cellular models of ALS. Motor neurons are recreated from skin cells obtained from people with ALS and healthy controls. Then, these cells are characterized and compared in hopes to identify differences called “phenotypes” that resemble key aspects of the disease.
The idea: to identify potential ALS medicines, cook up diseased motor neurons in the laboratory and then screen for drugs that remedy them.
“It has been a little frustrating that there have been a number of therapies that have been discovered in preclinical models of disease that haven’t had a demonstrable effect in clinical trials,” says University of California San Francisco (UCSF) neurologist Steven Finkbeiner MD PhD. “By using human neurons, particularly ones from patients with disease, perhaps we will have a model that will give us more relevant insights into the disease that can also be useful for finding small molecules that could have a therapeutic effect.”
Now, researchers from Kyoto University in Japan report the development of an induced pluripotent stem (iPS) cell-based screening platform that could be used to discover potential medicines for ALS.
The results come at the heels of a previous US UK study in which scientists including Steven Finkbeiner MD PhD demonstrated that motor neurons could be recreated in the laboratory that exhibited tell-tale signs of the disease.
Together, these studies pave the way toward the use of patient-derived iPS cell lines as a tool to discover new drugs for ALS.
“[We] hope these phenotypes could be a target to screen,” Kyoto University neuroscientist Haruhisa Inoue MD PhD leader of the study, writes ALS Today. ”We feel further scientific progress/technical advances [however] would be required.”
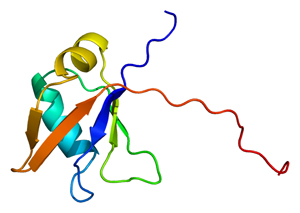
ALS in a dish. Researchers recreated motor neurons from people with an inherited form of ALS linked to a mutation in the transcription factor TDP-43. Image: Emw, Wikimedia Commons.
The findings are published this month in Science Translational Medicine.
The Kyoto University-based team created iPS cell lines from three ALS patients and seven healthy people and pushed them into motor neuron mode.
The researchers found that motor neurons generated from people with ALS appeared to be similar to those in the throws of the disease. The motor neurons accumulated clumps of TDP-43 protein in their cytoplasm. And, the nerve-like cells appeared to be more vulnerable to oxidative stress.
The team then treated motor neurons with four chemicals to assess their potential usefulness in identifying drugs for ALS. The team found that treatment with one chemical, anacardic acid, dropped levels of TDP-43 – largely in the cytoplasm – by nearly 150 fold.
The findings, together, suggest that this so-called screening platform could be potentially used to discover new drugs for the disease.
It pays to be the same
Key challenges however must be addressed before iPS-based screens can become routine 'drug discovery' practice. Motor neurons can take up to 2 months to create in the laboratory. What's more, iPS-based screens can be expensive: nearly three to five times that of conventional mouse screens according to Steven Finkbeiner MD PhD. But the biggest challenge drug discoverers and developers face is variability.
Researchers remain unsure how big a screening platform is needed to truly capture the heterogeneity of the disease. How many people with ALS need to be recruited? How many cell lines ultimately need to be screened particularly in regards to identifying medicines for sporadic disease?
Motor neurons reborn Scientists recreate motor neurons from people with ALS by pushing iPS cells into motor neuron mode. Here, healthy mouse motor neurons are generated. Video: SBI Biosystems.
Scientists around the world are working hard to create batteries of iPS cell lines from people with ALS in hopes to identify key cell lines that represent subsets of disease and at the same time, to control for differences in genetic backgrounds.
Furthermore, scientists remain unsure which iPS cell lines generate motor neurons that resemble those in each individual case of ALS. iPS cell lines originating from the same person with ALS can differ due to differences in degrees of reprogramming or other changes that occur due to culture conditions.
To meet the so-called clonal variability challenge, UCSF researchers are developing single iPS cell-based assays that can be used to measure benefits of potential ALS medicines in individual motor neurons over time. “We are kind of treating the cells like patients. Each cell serves as its own control,” explains Steven Finkbeiner MD PhD. “That seems to have helped quite a bit with variability.”
Meanwhile, the Kyoto University-based team, according to Harushisa Inoue MD PhD, is working hard to create better methods to create more consistent iPS cells that produce sufficient motor neurons for screening purposes.
Looking ahead, scientists anticipate that these strategies may not only help identify new potential medicines but in addition help identify those people with ALS that are likely to benefit from them - including those with sporadic disease.
“Without being able to pinpoint a genetic mutation, we may nevertheless be able to identify, sub-divide patients based on their cell physiology to drive the choice of medicines,” says Steven Finkbeiner MD PhD. “Instead of measuring blood pressure, we may be measuring protein homeostasis or some other internal pathway that may be a common thread in these diseases.”
To find out more about how scientists hope to use stem cells to better understand why motor neurons degenerate in people with ALS, read ALS motor neurons made easy?. To learn more about the challenges bringing stem cell-based treatment strategies into the clinic, check out Neuralstem: surging immunosuppression? and Operation Neuroprotection.
References
Egawa, N. et al. (2012) Drug screening for ALS using patient-specific induced pluripotent stem cells. Science Translational Medicine 4(145), 1-8. Abstract | Full Text (Subscription Required)
Bilican, B. et al. (2012) Mutant induced pluripotent stem cell lines recapitulate aspects of TDP-43 proteinopathies and reveal cell-specific vulnerability. Proceedings of the National Academy of Sciences, doi:10.1073/ pnas.1202922109. Abstract | Full Text (Open Access)
Further Reading
Son, E.Y., Ichida, J.K., Wainger, B.J., Toma, J.S., Rafuse, V.F., Woolf, C.J. and Eggan, K. (2011). Conversion of mouse and human fibroblasts into functional spinal motor neurons. Cell Stem Cell, 9(3), 205-218. Abstract | Full Text
Dimos, J.T. et al. (2008) Induced pluripotent stem cells generated from patients with ALS can be differentiated into motor neurons. Science 321, 1218-1221. Abstract | Full Text (Subscription Required)