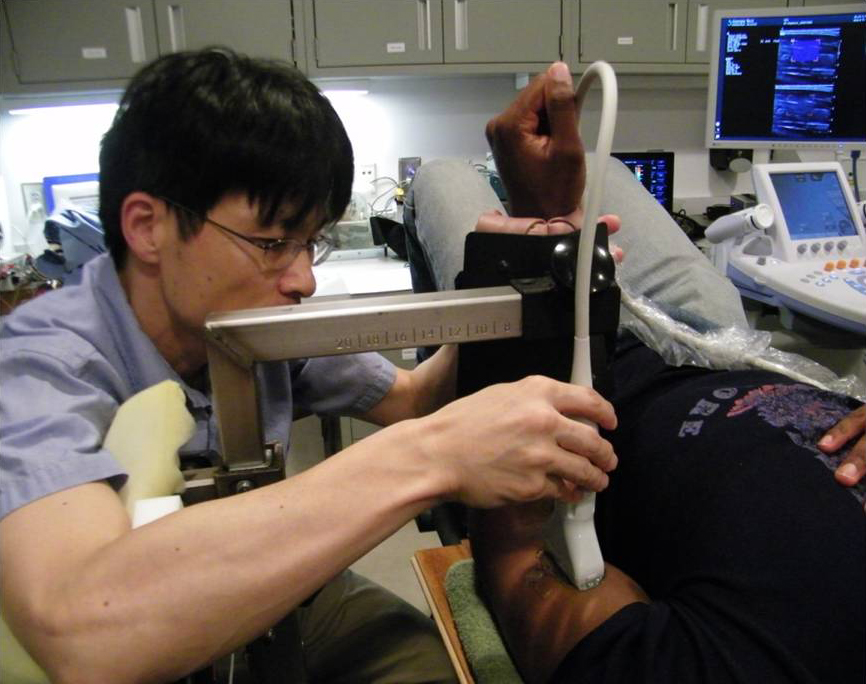
Sounding out NMJs A growing number of neurologists are looking to ultrasound in hopes to deduce the integrity of muscle-nerve connections. Image: Georgia Institute of Technology.
More than 30 potential ALS medicines are being tested in the clinic. But many people do not have access to them – waiting instead for a definitive diagnosis of disease.
A growing group of neurologists hopes to change that by turning to electrophysiological methods including electromyography (EMG) to check for subclinical signs of ALS.
The strategy, based on “Awaji criteria”, helps clinicians solidify the diagnosis of ALS by checking the muscles for twitches (fasciculations) – an early sign of the disease. The technique by some estimates might increase the number of people eligible for clinical trials by 25%.
But checking muscles by EMG can hurt. And, the test can sometimes miss key signs of disease.
Some clinicians suspect that ultrasound can enable them to peer into the muscles of people with suspected ALS. And, confirm whether their patients have the disease.
The non-invasive technique, known as neuromuscular ultrasound (NMUS), might identify key signs of ALS in the muscles and motor nerves. And, check if the muscles contract properly - without the pain of EMG.
A clinical trial at Duke University School of Medicine is now ongoing.
"We are trying to see how the two compare - to see how good ultrasound might be diagnostically," says principal investigator Lisa Hobson-Webb MD.
Pumping up ALS diagnosis
Wake Forest University School of Medicine neurologist Francis Walker MD turned to NMUS in the 1980s in hopes to better diagnose neuromuscular disease. The technique, he reasoned, could enable clinicians to evaluate larger areas of muscles for signs of atrophy and weakness. And, check their function.

Spacing the needles Clinicians hope to reduce the number of muscles that need to be tested by electromyography (EMG) by checking first via NMUS for key signs of disease. Image: Joe Stevens, Gruenrekorder.
Reporting in 1990, he found that NMUS appeared to outperform EMG in identifying fasciculations in people with diseases neuromuscular in nature – including 2 people with ALS.
The technique according to more recent studies led by Chiba University Hospital neurologist Satoshi Kuwabara MD appears to detect twitches in 98% of people with ALS – 10% more than EMG.
What’s more, NMUS appears to enable clinicians to diagnose more people suspected to have the disease. Nearly 80% of people were diagnosed with either probable or definite ALS – twice the number identified via El Escorial criteria using conventional methods. And, 5% more via Awaji criteria using EMG.
The results suggest that NMUS may enable more people to be diagnosed – enabling them to participate in clinical trials of medicines earlier in their course of disease.
Getting the nerve
With the advent of higher resolution ultrasound machines, clinicians began to examine the peripheral nerves of people with ALS for additional signs of the disease.
Some signs of atrophy could be detected in a key motor nerve in people with ALS according to a 2011 study led by Wake Forest’s Michael Cartwright MD. But a key sensory nerve remained unaffected. A nerve untouched by the disease.
The results suggested that tell tale changes in the size of the motor nerves alone might help identify people with ALS.
And, according to Michael Cartwright MD, also help rule out key disorders often confused with the disease. Motor nerves typically become bigger in people with chronic inflammatory demyelinating polyneuropathy (CIDP) and multifocal motor neuropathy (MMN). In people with ALS, the motor nerves slightly shrink.
Now, Duke University School of Medicine clinicians are putting NMUS to the test to determine whether the technique can be used to identify people with ALS - strongly suspected to have the disease. Muscles in the arms, legs and tongue will be checked for signs of atrophy and weakness (increased fibrosis). And, the nerves in the arms and legs will be checked for signs of axonal damage (reduced size).
All participants will be examined by NMUS on a periodic basis for one year to determine if these signs can also be used to monitor the disease.
“I think the bigger promise in ultrasound is in clinical trials. I think it could really help in clinical trial design,” says Duke University School of Medicine’s Lisa Hobson-Webb MD.
A clinical trial is ongoing. The study is in collaboration with neurologist Rick Bedlack MD, Director of the Duke ALS Clinic. 50 people with suspected ALS are expected to participate.
A brighter future
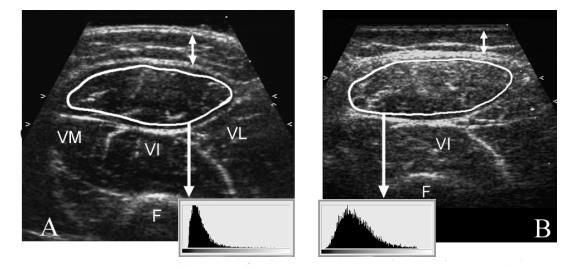
And the muscles echoed Clinicians look at muscles by NMUS for signs of fibrosis (bright speckles) – a key contributor of muscle weakness. Here, ultrasounds of leg muscles of a healthy person (A) and a person with Duchenne muscular dystrophy are shown. Image: Sigrid Pillen MD, UMC St Radboud Medical Centre, The Netherlands. Courtesy of PAGE Press.
UMC St Radboud University Nijmegen Medical Centre neurophysiologist Sigrid Pillen MD PhD turned to NMUS in the early 2000s to help identify young people with neuromuscular disease. Her strategy, which involved looking for changes in muscle architecture, appeared to help identify children with key neuromuscular disorders including Spinal Muscular Atrophy and Friedrich’s Ataxia. And, distinguish them from those with other muscle or nerve diseases (myopathies or neuropathies) at about 90% accuracy.
UMC St Radboud neurologists suspected that these same techniques could be used to improve the diagnosis of ALS. Reporting in 2008, the clinicians found that NMUS appears to identify key signs of muscle atrophy and weakness (increased fibrosis). And, spot twitches in most people with ALS - confirming observations by Wake Forest University School of Medicine's Francis Walker MD.
In 2012, the team proposed a new strategy to increase the certainty of diagnosis of ALS. The plan: identify fasciculations in at least four muscles. And, increased fibrosis (muscle echogenicity) in two muscles. The technique appears to identify people with ALS at about 96% accuracy. And, rule out ALS, 84%.
Now, a growing number of neurophysiologists are using combined methods to identify people with ALS. The strategy reduces the number of muscles that need to be checked using electrophysiological methods – including EMG. EMG however is still needed according to Wake Forest School of Medicine's Michael Cartwright MD to determine whether the condition is primarily a nerve disease.
“We use ultrasound to increase the certainty of diagnosis. And, exclude other disorders,” explains Wake Forest School of Medicine’s Michael Cartwright MD.
But whether NMUS alone can be used to increase the certainty of ALS diagnosis remains an open question according to Hannover Medical School's Reinhard Dengler MD.
NMUS may be able to distinguish people with ALS from other outwardly similar disorders including hereditary spastic paraparesis (HSP) according to a study led by UMC St Radboud's Jurgen Schelhaas MD. But other conditions including Kennedy’s disease and multifocal motor neuropathy (MMN) remain untested. Key disorders often confused with the disease.
And, the tests need to be standardized according to Duke University School of Medicine's Lisa Hobson-Webb MD. Sonographers can spot changes in the size of muscles. But estimating the degree of fibrosis (muscle echogenicity) is trickier. The measures can differ from person to person. And, machine to machine.
Multi-center trials are needed to rigorously evaluate NMUS in the ALS clinic. And, to develop standardized guidelines to implement NMUS in general practice.
Clinicians nevertheless remain confident that the technology holds great benefit for people with ALS.
"Ultrasound could be an excellent tool to reduce invasive testing," says Duke University School of Medicine's Lisa Hobson-Webb MD, "and increase the power of clinical trials."
***
To learn more about how clinicians currently diagnose the disease, check out What is ALS? To find out about other non-invasive strategies being developed to diagnose ALS, check out TMS, a headstart for PALS? and MRI, Make that a Double.
Patient Resources
Neuromuscular ultrasound in ALS Contact | ALS TDI | Website
Video: What to expect during a Nerve conduction study and EMG Youtube
References
Cartwright, M.S., Walker, F.O., Griffin, L.P. and Caress, J.B. (2011) Peripheral nerve and muscle ultrasound in amyotrophic lateral sclerosis. Muscle & Nerve 44(3), 346-351. Abstract | Full text
Arts, I.M., Overeem, S., Pillen, S., Schelhaas, H.J. and Zwarts, M.J. (2011) Muscle ultrasonography to predict survival in amyotrophic lateral sclerosis. Journal of Neurology, Neurosurgery and Psychiatry 82(5), 552-554. Abstract | Full text (Subscription Required)
Arts, I.M., van Rooij, F.G., Overeem, S., Pillen, S., Janssen, H.M., Schelhaas, H.J. and Zwarts, M.J. (2008) Quantitative muscle ultrasonography in amyotrophic lateral sclerosis. Ultrasound in Medicine and Biology 34(3), 354-361. Abstract | Full text (Subscription Required)
Further Reading
Padua, L. and Hobson-Webb, L.D (2013) Ultrasound as the first choice for peripheral nerve imaging? Neurology 80(18), 1626-1627. Abstract | Full text (Subscription Required)
Hobson-Webb, L.D. (2013) Neuromuscular ultrasound in polyneuropathies and motor neuron disease. Muscle & Nerve 47(6), 790-804. Abstract | Full text (Subscription Required)
Mayans, D., Cartwright, M.S. and Walker, F.O. (2012) Neuromuscular ultrasonography: quantifying muscle and nerve measurements. Physical Medicine and Rehabilitation Clinics of North America 23(1), 133-148. Abstract | Full text